The Ramalingaswami Centre on Equity & Social Determinants of Health (“Centre”) was set up in Bangalore in 2015, as a Centre of Excellence at the Public Health Foundation of India (PHFI). Since then, it has become a go-to place for training, research and knowledge translation on gender and intersectionality in health systems and policy.
The team at the Centre has an excellent track record of in-depth grounded research straddling different methodologies.
Over the years, its members have:
- Challenged existing conceptual frameworks in maternal health
- Developed new methodological approaches to verbal autopsies and intersectionality-focused analyses
- Linked key health system factors to gender dynamics to better understand the drivers of maternal mortality and respectful maternity care
- Explored the role of power in health systems
- Developed equity-oriented strategies to engage diverse health system stakeholders
- Taken an intersectionality lens to public policy
The Centre has also engaged with key national and international health policy bodies (Mission Steering Group of the NRHM, governing board of the NHSRC, Scientific and Technical Advisory Group and Gender and Rights Advisory Panel of WHO’s RHR / HRP department and more). Over the years, the Centre has built up collaborative partnerships with institutions and universities globally, and within India – National Institute of Mental Health and Neuro Sciences (NIMHANS), Indian Institute of Public Health, Shillong, United Nations University- International Institute of Global Health (UNU-IIGH), University of Toronto’s Centre for Global Child Health, Federal University of Pelotas’ International Centre for Equity in Health, University of Western Cape, George Washington University’s Milkin School of Public Health and its members are affiliated to networks like Health Equity Network India, CommonHealth, etc.
Our funders have included WHO’s Alliance for Health Policy and Systems Research, WHO’s Department of RHR/HRP, UNFPA, UNU-IIGH, the Bill and Melinda Gates Foundation, World Bank, & Nilekani Philanthropies.
Mission
The mission of the Ramalingaswami Centre on Equity and Social Determinants of Health is to contribute to efforts to improve the health of India’s population by reducing health inequalities, focusing particularly on socioeconomically disadvantaged groups.
Aims

The Centre’s aims are four-fold:
- To conduct cutting-edge, grounded, in-depth primary research and reviews on equity and the social determinants of health with a strong focus on gender and its intersections with other sources of socioeconomic power.
- To develop teaching materials grounded in field experiences and research on socio-economic inequality to strengthen public health training in India.
- To foster linkages between researchers, programme implementers and policymakers to support evidence-based policy development.
- To create knowledge products that promote active engagement with public health concerns by a wide range of stakeholders.
Workstreams
Research
Disrespect and abuse (D&A) in obstetric care are recognised as a widespread and systemic problem. Quantitative, qualitative and intervention research aimed at understanding and addressing it better has pointed to the root causes of D&A within socio-economic inequality or within power hierarchies in health care provision. But there has been relatively little attempt to identify and document the actual mechanisms through which power relations translate into health care practices or behaviours. Such an effort is essential if one is to appreciate why D&A in maternal care are so widespread, and how the problem might be addressed effectively.
The centre has conducted both qualitative and quantitative research in southern India to better understand the phenomena of disrespectful and abusive in obstetric care and family planning services.
- Maternal Clinical Assessment Tool (M-CAT): This was a proof-of-concept study, leveraging digital technology to improve the quality of antepartum and postpartum clinical assessments.
- A cross-sectional community survey was designed to meet two objectives:
- To understand rural women’s perceptions and experience of institutional obstetric care, including the strategies used to negotiate better care, and
- To measure and explain differences in perceptions of institutional obstetric care by social location of the woman, type of institution, and stage of the village’s transition to institutional birth.
- Qualitative research with healthcare providers: The focus of our qualitative research was to explore the causes of obstetric care-linked D&A in healthcare institutions, especially the role of professional training and work cultures. Our questions were: (1) To what extent does routine obstetric practice vary from available protocols and guidelines, and why? (2) Where do these practices come from? Do they lie in insufficient training? Are these practices picked up during internships and residencies?
- A scoping review of organisational conditions and their impact on maternity providers and care in LMICs: Implications for Respectful Maternity Care
We are currently engaged in formative research on women’s health and well-being in collaboration with University of Toronto’s Centre for Global Child Health, UNFPA, Federal University of Pelotas’ International Centre for Equity in Health, and George Washington University’s Milkin School of Public Health. This cutting-edge work combines a life course approach with a gender and intersectionality lens and focuses on conceptual advancement along with metrics and dashboards to track progress on women’s health and well-being.
The Centre is conducting formative research into the growing health challenges in urban India, with a specific focus on the vulnerabilities of particular marginal groups, using an intersectional lens. The definition of the ‘urban’ is in itself complicated, particularly in the Indian context, where it could mean anything from a metro city to a district headquarters town. Each of these urban centres has a governance structure and a health system peculiar to its history and development trajectory. Also, urban poverty and marginality are multidimensional and layered, and often invisible. Despite this complexity, information around urban health is sparse. The Centre aims to bridge this gap through a focused workstream on urban health issues.
Training/Teaching/Mentoring

- The Centre successfully ran a fellowship programme aimed at strengthening gender equity and intersectionality in health policy and systems research. The centre was selected as RMI by WHO’s Alliance for Health Policy and Systems Research. The programme was run in collaboration with the United Nations University – International Institute for Global Health (UNU-IIGH).
- This resulted in a high-quality modular online course emphasising case-based learning, ready to be rolled out in multiple settings.
- The Centre is also planning several short duration courses on Research Methodology and Patient Centred Communication for Health Professionals, among others.
Policy Engagement
The Centre engages in policy development at three levels: local/state, national and global.
- At the state level, we are collaborating with the World Bank to look at ways in which the Government of Tamil Nadu could address challenges to the (sexual, reproductive, nutritional, and mental) health of adolescents.
- At the national level, we are researching the functioning of publicly funded health insurance schemes: Are all enrolled families below the poverty line (BPL)? Which BPL families get excluded? Are the schemes sensitive to power relations and distributional challenges within and across households? How might these challenges be addressed?
- Globally, the Centre has been actively engaged, in collaboration with UNU-IIGH, University of the Western Cape and WHO-SEARO, in developing recommendations for sustainable interventions that integrate gender into government health programs. Titled ‘Promising Practices in Integrating Gender into Government Health Programs’, the project looks at what works and what doesn’t in three global regions – Africa, Southeast Asia and South Asia. What lessons can we learn from government health programmes that take gender integration seriously?

Publications
Rao, A., Srinidhi, V., Karachiwala, B., Santosh, S., Seshadri, S. R., Thomas, S., … & Sen, G. (2024). How power and knowledge hierarchies affect communication in intrapartum care: findings from public health facilities in two southern Indian districts. BMC Pregnancy and Childbirth, 24(1), 781.
Bohren, M. A., Iyer, A., Barros, A. J. D., Williams, C. R., Hazfiarini, A., Arroyave, L., Filippi, V., Chamberlain, C., Kabakian-Khasholian, T., Mayra, K., Gill, R., Vogel, J. P., Chou, D., George, A. S., & Oladapo, O. T. (2024). Towards a better tomorrow: Addressing intersectional gender power relations to eradicate inequities in maternal health. eClinicalMedicine, 67.
https://doi.org/10.1016/j.eclinm.2023.102180
Reddy, B., Thomas, S., Karachiwala, B., Sadhu, R., Iyer, A., Sen, G., Mehrtash, H., & Tunçalp, Ö. (2022). A scoping review of the impact of organisational factors on providers and related interventions in LMICs: Implications for respectful maternity care. PLOS Global Public Health, 2(10), e0001134.
https://doi.org/10.1371/journal.pgph.0001134
Srinidhi, V., Karachiwala, B., Iyer, A., Reddy, B., Mathrani, V., Madhiwalla, N., Periodi, V., Sreevathsa, A., Viswanatha, L., & Sen, G. (2021). ASHA Kirana: When digital technology empowered front-line health workers. BMJ Global Health, 6(Suppl 5), e005039.
https://doi.org/10.1136/bmjgh-2021-005039
Sen, G., Reddy, B., Iyer, A., & Heidari, S. (eds) (2018), “Disrespect and abuse in maternal care: Addressing key challenges”, Special Issue of Reproductive Health Matters, 26 (53): 1-129,
DOI: https://doi.org/10.1080/09688080.2018.1525176
Sen, G., Reddy, B., & Iyer, A. (2018). Beyond measurement: The drivers of disrespect and abuse in obstetric care. Reproductive Health Matters, 26(53), 6–18.
https://doi.org/10.1080/09688080.2018.1508173
Sen, G., Reddy, B., Iyer, A., & Heidari, S. (2018). Addressing disrespect and abuse during childbirth in facilities. Reproductive Health Matters, 26(53), 1–5.
https://doi.org/10.1080/09688080.2018.1509970
Iyer, A., Srinidhi, V., Sreevathsa, A., & Sen, G. (2017). Adapting maternal health practice to co-morbidities and social inequality: A systematic approach. Canadian Journal of Public Health / Revue Canadienne de Santé Publique, 108(4), e448–e451. DOI: https://doi.org/10.17269/cjph.108.5571
Schaaf, M., Boydell, V., Topp, S. M., Iyer, A., Sen, G., & Askew, I. (2022). A summative content analysis of how programmes to improve the right to sexual and reproductive health address power. BMJ Global Health, 7(4), e008438. https://doi.org/10.1136/bmjgh-2022-008438
Sen, G., Iyer, A., Chattopadhyay, S., & Khosla, R. (2020). When accountability meets power: Realizing sexual and reproductive health and rights. International Journal for Equity in Health, 19(1), 111.
https://doi.org/10.1186/s12939-020-01221-4
Sen, G., Kismödi, E., & Knutsson, A. (2019). Moving the ICPD agenda forward: Challenging the backlash. Sexual and Reproductive Health Matters, 27(1), 319–322.
https://doi.org/10.1080/26410397.2019.1676534
Correa, S., Germain, A., & Sen, G. (2016). Feminist mobilizing for global commitments to the sexual and reproductive health and rights of women and girls. In E. Chesler & T. McGovern (Eds.), Women and Girls Rising: Progress and Resistance Around the World (pp. 51-68). New York, USA: Taylor& Francis.
DOI: https://doi.org/10.4324/9781315708379-5
Srinidhi, V., Iyer, A., Sreevathsa, A., & Shankar, M. (2016). Translating Research into a Capacity-Building Tool to Strengthen Obstetric Competence. BMJ Global Health, 1:A26.
https://doi.org/10.1136/bmjgh-2016-EPHPabstracts.34
Germain, A., Sen, G., Garcia-Moreno, C., & Shankar, M. (2015). Advancing sexual and reproductive health and rights in low- and middle-income countries: Implications for the post-2015 global development agenda. Global Public Health, 10(2), 137–148.
https://doi.org/10.1080/17441692.2014.986177
Sen, G., & Govender, V. (2015). Sexual and reproductive health and rights in changing health systems. Global Public Health, 10(2), 228–242.
https://doi.org/10.1080/17441692.2014.986161
Sen, G., Germain, A., Garcia-Moreno, C., & Shankar, M. (Guest Eds) (2015) Sexual and Reproductive Health and Rights for the next decades: What’s been achieved? What lies ahead? Global Public Health 10(2).
https://www.tandfonline.com/toc/rgph20/10/2
Martopullo, I., Neves, P. A., Baird, S., Liang, M., Keats, E. C., Cherkas, A., … & Bhutta, Z. A. (2024). Understanding progress and challenges in women’s health and wellbeing in exemplar countries: a time-series study identifying positive outliers. The Lancet Global Health, 12(12), e2012-e2023.
Iyer, A., & Sen, G. (2020). Unjust social differences: Health inequalities in India. In A. Mehdi & I. Rajan (Eds.), Health of the nation: Perspectives for a new India (pp. 86-100). New Delhi: Oxford University Press.
https://india.oup.com/product/health-of-the-nation-9780199499830
Sen, G., & Iyer, A. (2019). Beyond economic barriers: Intersectionality and health policy in low- and middle-income countries. In O. Hankivsky & J. Jordan-Zachery (Eds.), The Palgrave Handbook of Intersectionality in Public Policy (pp. 245-261). Palgrave Macmillan.
https://www.academia.edu/81464343/The_Palgrave_Handbook_of_Intersectionality_in_Public_Policy?f_ri=34327
Sen, G., & Iyer, A. (2016). The Mechanisms of Intersectioning Social Inequalities in Health. BMJ Global Health, 1(Suppl 1).
https://doi.org/10.1136/bmjgh-2016-EPHPabstracts.47
Mason, E., Sen, G., & Yamin, A. E., on behalf of the United Nations Secretary-General’s Independent Accountability Panel for Every Woman, Every Child, E. A. (2020). Ensuring UHC protects the health and rights of women, children and adolescents. Accelerating Universal Health Coverage, Bulletin of the World Health Organization (Theme Issue), 98(2), 79-79A.
https://doi.org/10.2471/BLT.19.249474
Sen, G., Virani, A., Iyer, A., Reddy, B., & Selvakumar, S. (2017). Translating health research to policy: Breaking through the impermeability barrier. In J. Georgalakis, N. Jessani, R. Oronje, & B. Ramalingam (Eds.), The Social Realities of Knowledge for Development (pp. 32–51). Brighton: IDS Impact Initiative.
https://www.researchgate.net/publication/320212414_Translating_Health_Research_to_Policy_Breaking_through_the_Impermeability_Barrier
Sen, G., & Iyer, A. (2015). Health policy in India: some critical concerns. In E. Kuhlmann, R. H. Blank, & I. L. Bourgeault (Eds.), The Palgrave International Handbook of Healthcare Policy and Governance (pp. 154–170). Hampshire: Palgrave Macmillan.
https://link.springer.com/book/10.1057/9781137384935
Seshadri, S. R. (2022). The Covid-19 Pandemic and the Health Sector: What have we learned? In School of Policy and Governance in association with the Constitutional Conduct Group (Ed.), Understanding Post-Covid 19 Governance Challenges in India. Azim Premji University.
https://azimpremjiuniversity.edu.in/publications/2022/report/understanding-post-covid-19-governance-challenges-in-india
Fisseha, S., Sen, G., Ghebreyesus, T. A., Byanyima, W., Diniz, D., et al. (2021). COVID-19: The turning point for gender equality. The Lancet, 398(10299), 471–474.
https://doi.org/10.1016/S0140-6736(21)01651-2
Promising Practices in Integrating Gender into Government Health Programs’ project was a collaborative effort between PHFI’s Ramalingaswami Centre on Equity and Social Determinants of Health (RCESDH-PHFI), United Nations University International Institute for Global Health (UNU-IIGH),and the School of Public Health at the University of Western Cape in South Africa. The project aimed to bridge the critical evidence gap regarding successful integration of gender into large-scale government health programs, through a series of national case studies.
The resultant case study series consists of three stand-alone summaries with key findings spanning policy, systems, institutional, and community levels.
Beneria, L., & Sen, G. (2021). Feminist economic challenges to development. In I. Berik & E. Kongar (Eds.), The Routledge Handbook of Feminist Economics. Taylor & Francis.
https://www.routledge.com/The-Routledge-Handbook-of-Feminist-Economics/Berik-Kongar/p/book/9780367074142
In the News
Resources
Commission on Social Determinants of Health Knowledge Networks et al. (2011) Improving Equity in Health by Addressing Social Determinants, Geneva: WHO
http://apps.who.int/iris/bitstream/10665/44793/1/9789241503037_eng.pdf
Sen, Gita and Ostlin, Piroska (2011) Gender inequity in health, In Improving Equity in Health by Addressing Social Determinants Geneva, WHO, 2011
http://apps.who.int/iris/bitstream/10665/44793/1/9789241503037_eng.pdf
Sen, Gita and Ostlin, Piroska (2011) Priorities for research on equity and health: Towards an equity-focused health research agenda in PLoS Medicine, November, 8 (11): e1001115 (doi:10.1371/journal.pmed.1001115) (selected for the special WHO/PLoS collection, “World Health Report 2012: No Health Without Research”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3206017/pdf/pmed.1001115.pdf
Sen, Gita and Ostlin, Piroska (2011) Gender based inequities in global public health in Richard Parker and Marni Sommer (Eds) The Routledge International Handbook on Global Public Health, Routledge
https://www.routledge.com/Routledge-Handbook-of-Global-Public-Health/Parker-Sommer/p/book/9780415818896
Sen, Gita and Ostlin, Piroska (Eds) (2010) Gender Equity in Health: The Shifting Frontiers of Evidence and Action, New York: Routledge Studies in Health and Social Welfare
https://www.routledge.com/Gender-Equity-in-Health-The-Shifting-Frontiers-of-Evidence-and-Action/Sen-Ostlin/p/book/9780415654937
Sen, Gita and Ostlin, Piroska (2010) Gender as a Social Determinant of Health –Evidence, Policies and Innovations In Gita Sen and PiroskaOstlin (Eds) Gender Equity in Health: the Shifting Frontiers of Evidence and Action, New York, Routledge Studies in Health and Social Welfare (Abridged version published in N Visvanathan, L Duggan, N Wiegersma and L Nisonoff Eds. 2011 The Women, Gender and Development Reader, London: Zed Books, 2nd edition)
https://www.routledge.com/Gender-Equity-in-Health-The-Shifting-Frontiers-of-Evidence-and-Action/Sen-Ostlin/p/book/9780415654937
Sen, Gita (2009) Health inequalities: gendered m and conundrums. The 10th Annual Sol Levine lecture Social Science and Medicine, October, 69 (7): 1006-1009
http://dx.doi.org/10.1016/j.socscimed.2009.07.027
Sen, Gita and Ostlin, Piroska (2008) Gender inequity in health: Why it exists and how we can change it, Global Public Health 3(2): Supplement 1, 1-12; reprinted in Richard Hofrichter and Rajiv Bhatia (Eds) 2010 Tackling Health Inequities through Public Health Practice –Theory to Action, New York: Oxford University Press, (Second Edition).
http://www.tandfonline.com/doi/full/10.1080/17441690801900795?scroll=top&needAccess=true
Sen, Gita and Ostlin, Piroska (Eds) (2008) Gender Inequity in Health: Why It Exists and How We Can Change It Special Supplement, Global Public Health 3 (2): Supplement 1
http://www.tandfonline.com/doi/full/10.1080/17441690801900795
Sen, Gita, Ostlin, Piroska and George, Asha (2007) Unequal, unfair, ineffective and inefficient: Gender inequity in health – Why it exists and how we can change it, Final report to the WHO Commission on Social Determinants of Health by the Women and Gender Equity Knowledge Network
http://www.who.int/social_determinants/resources/csdh_media/wgekn_final_report_07.pdf
Sen, Gita, Iyer, Aditi and George, Asha (2007) Systematic hierarchies and systemic failures: gender and health inequities in Koppal district Economic and Political Weekly, February 24-March 2, XLII (8): 682-690; and in Gopal Kadekodi, Ravi Kanbur and Vijayandra Rao (Eds.) Development in Karnataka: Challenges of Governance, Equity and Empowerment, New Delhi: Academic Press, 357-382
https://www.researchgate.net/publication/262698396_Systematic_hierarchies_and_systemic_failures_Gender_and_ health_inequities_in_Koppal_District
Sen, Gita, George, Asha and Ostlin, Piroska (Eds) (2002) Engendering International Health: the Challenge of Equity, Cambridge: The MIT Press
https://mitpress.mit.edu/books/engendering-international-health
Intersecting inequalities
Iyer, Aditi, Sen, Gita and Ostlin, Piroska (2010) Inequalities and intersections in health: a review of the evidence In Gita Sen and PiroskaOstlin (Eds) Gender Equity in Health: the Shifting Frontiers of Evidence and Action New York: Routledge Studies in Health and Social Welfare.
https://www.routledge.com/Gender-Equity-in-Health-The-Shifting-Frontiers-of-Evidence-and-Action/Sen-Ostlin/p/book/9780415654937
Iyer, Aditi, Sen, Gita and Ostlin, Piroska (2008) The intersections of gender and class in health status and health care In Gita Sen and PiroskaOslin (Eds) Gender Inequity in Health: Why It Exists and How We Can Change It, Global Public Health, 3(2): Supplement 1.
http://www.tandfonline.com/doi/full/10.1080/17441690801892174
Iyer, Aditi, Sen, Gita and George, Asha (2007) The dynamics of gender and class in access to health care: evidence from rural Karnataka, India International Journal of Health Services, 37 (3): 537–554.
https://jhu.pure.elsevier.com/en/publications/the-dynamics-of-gender-and-class-in-access-to-health-care-evidenc-4
Sen, Gita and Iyer, Aditi (2016), “The mechanisms of intersecting social inequalities in health”, BMJ Global Health 2016; 1(Suppl 1): A35-A36
http://gh.bmj.com/content/1/Suppl_1/A35
Sen, Gita and Iyer, Aditi (2012) “Who gains, who loses and how: Leveraging gender and class intersections to secure health entitlements”, Social Science and Medicine 72: 1802-1811
http://www.sciencedirect.com/science/article/pii/S0277953611003236
Sen, Gita, Iyer, Aditi and Mukherjee, Chandan (2009) “A methodology to analyse the intersections of social inequalities in health”Journal of Human Development and Capabilities, 10 (3): 397–415
http://www.tandfonline.com/doi/full/10.1080/19452820903048894?scroll=top&needAccess=true
Jacob, S and Chattopadhyay, S (2019) Speaking of Abuse: The Pyramid of Reporting Domestic Violence in India. Economic and Political Weekly. 54(1): 53-63. Chattopadhyay, S. (2018). The shifting axes of marginalities: the politics of identities shaping women’s experiences during childbirth in Northeast India. Reproductive Health Matters, 1–8.
https://doi.org/10.1080/09688080.2018.1502022
[Taylor and Francis]. Chattopadhyay, S. (2018) The responses of health systems to marital sexual violence – a perspective from southern India. In Aggression, Maltreatment and Trauma. Doi:
https://doi.org/10.1080/10926771.2018.1494235
[Taylor and Francis] Chattopadhyay, S., Mishra, A., Jacob, S. (2017) Safe Yet Violent: Women’s Experiences with Obstetric Violence during Hospital Births in Rural Northeast India in Culture, Health and Sexuality.
https://doi.org/10.1080/13691058.2017.1384572
[Taylor and Francis] Correa S, Germain A, Sen G. (2016) Feminist mobilizing for global commitments to the sexual and reproductive health and rights of women and girls. In: Chesler E, McGovern T editors. Women and Girls Rising: Progress and Resistance Around the World, New York, USA: Routledge; 51-68
https://www.routledge.com/Women-and-Girls-Rising-Progress-and-resistance-around-the-world/Chesler-McGovern/p/book/9781138898776
George, Asha, Iyer, Aditi and Sen, Gita (2005) Maternity in crisis: Gendered health system experiences from Koppal, Karnataka IDS Sussex Working Paper No 253, Brighton, Sussex: Institute of Development Studies, September.
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.605.2179&rep=rep1&type=pdf
Iyer, Aditi, Sen, Gita and Sreevathsa, Anuradha (2013). Deciphering Rashomon: An approach to verbal autopsies of maternal death Global Public Health: An International Journal for Research, Policy and Practice, 8 (4): 389-404.
http://www.tandfonline.com/doi/abs/10.1080/17441692.2013.772219
Iyer, Aditi, Sen, Gita, Sreevathsa, Anuradha and Varadan, Vasini (2012) Verbal autopsies of maternal deaths in Koppal, Karnataka: lessons from the grave BMC Proceedings, 6 (Suppl 1):P2
http://www.biomedcentral.com/1753-6561/6/S1/P2
Reddy, Bhavya, Sen, Gita (2013) Breaking Through the Development Silos. Sexual & Reproductive Health and Rights, Millennium Development Goals and Gender Equity: Experiences from Mexico, India and Nigeria, Reproductive Health Matters, 21(42): 18-31.
http://www.rhm-elsevier.com/article/S0968-8080(13)42743-X/pdf
Sen, Gita (2014) Sexual and reproductive health and rights in the post-2015 development agenda Global Public Health, 9 (6): 599-606
http://www.tandfonline.com/doi/full/10.1080/17441692.2014.917197
Sen, Gita (2013) Gender equality in the post 2015 development agenda: Lessons from the MDGs IDS Bulletin 44 (5-6), September: 42-48
http://onlinelibrary.wiley.com/wol1/doi/10.1111/1759-5436.12055/abstract
Sen, Gita (2010) Family Planning and Sexual and Reproductive Health and Rights: The Past as Prologue? Studies in Family Planning, June, 41 (2): 143-146
http://onlinelibrary.wiley.com/doi/10.1111/j.1728-4465.2010.00237.x/abstract
Sen, Gita, Govender, Veloshnee and Cottingham, Jane (2007) Maternal and neonatal health: surviving the roller-coaster of international policy, March, Occasional Paper Series Number 5, Centre for Public Policy, Indian Institute of Management Bangalore
http://www2.ids.ac.uk/ghen/resources/papers/MaternalMortality2006.pdf
Shankar, Mridula and Reddy, Bhavya (2012) Anaemia in pregnancy still a major cause of morbidity and mortality: Insights from Koppal district, Karnataka, India Reproductive Health Matters, 20 (40): 67-68 http://www.rhm-elsevier.com/article/S0968-8080(12)40669-3/abstract
Series on Decoding Maternal Safety
Ottersen, T., Norheim, O.F. et al. (including Gita Sen) (2014) Making fair choices on the path to universal health coverage, Final report of the WHO Consultative Group on Equity and Universal Health Coverage, Geneva: WHO
http://apps.who.int/iris/bitstream/10665/112671/1/9789241507158_eng.pdf
Ottersen, T., Norheim, O.F. et al. (including Gita Sen) (2014) Making fair choices on the path to universal health coverage, Bulletin of the World Health Organization, 92 (6), June: 389.
http://dx.doi.org/10.2471/BLT.14.139139
Reddy, K. Srinath et al (including Gita Sen) (2011) Report of the High Level Expert Group on Universal Health Coverage, Submitted to the Planning Commission of India
http://planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf
Sen, Gita (2014) Health security in Ashima Goyal (Ed) The Oxford Handbook of the Indian Economy in the 21st Century, New Delhi, Oxford University Press, pp 328-51 Sen, Gita (2012) Universal health coverage in India: a long and winding road Economic and Political Weekly February 25, XLVII (8): 45-52
http://uhc-india.org/uploads/GitaSen.pdf
Fostering Knowledge-Implementation Links Project (2012) Maternal Death Reviews:Improving the quality of evidence to support health system strengthening, Policy Brief No. 1 Bangalore: Indian Institute of Management Bangalore.
http://www.phfi.org/images/pdf/Knowledge-translation_policy_brief_1.pdf
Fostering Knowledge-Implementation Links Project (2012) Identification and management of obstetric risks and emergencies: How prepared are primary level providers? Policy Brief No. 2, Bangalore: Indian Institute of Management Bangalore.
http://www.phfi.org/images/pdf/Knowledge-translation_policy_brief_2.pdf
Fostering Knowledge-Implementation Links Project (2012) Programmatic strategies for tackling maternal anaemia: Lessons from research and experience. Policy Brief No. 3, Bangalore: Indian Institute of Management Bangalore.
http://www.phfi.org/images/pdf/Knowledge-translation_policy_brief_3.pdf
Fostering Knowledge-Implementation Links Project (2012) Pregnant women with moderate to Severe anaemia: Lacunae in screening and treatment efforts. Policy Brief No. 4, Bangalore: Indian Institute of Management Bangalore.
http://www.phfi.org/images/pdf/knowledge-translation_policy_brief_4.pdf
Srinidhi V, Iyer, Aditi, Sreevathsa, Anuradha and Shankar, Mridula (2016), “Translating research into a capacity-building tool to strengthen obstetric competence”, BMJ Global Health 2016; 1(Suppl 1): A26
http://gh.bmj.com/content/bmjgh/1/Suppl_1/A26.1.full.pdf
YAARA HONE?
Building collective responsibility for maternal safety
Download PDF
IDENTIFYING AND ASSESSING MATERNAL RISKS
A handbook for healthcare providers
Download PDF
ARIVU NERAVU FOR MATERNAL HEALTH
What communities should know and do
Download PDF
ASHA KIRANA: A Tool for Safer Pregnancy
A Status Report
2017
Download PDF
This film presents work done by the Ramalingaswami Centre on Equity and Social Determinants of Health on improving maternal health in poor rural areas. It documents the Maternal Clinical Assessment Tool (M-CAT), a project aiming to build the capacities of Accredited Social Health Activists (ASHAs) to support better clinical assessment of pregnant and postpartum women.
Set in Koppal, a district in the southern Indian state of Karnataka, the video captures what it means to be a woman in a poor rural area through the lens of the Gender and Equity (GHE) Project. In doing this, the film subtly reveals how transforming gender injustice also leads to taking a quiet stand against caste bias and other kinds of stigma. It tells an unfinished story of resilience and change.
There are so many Koppals in India. This film is dedicated to Koppal’s women wherever they may be.
The monthly Colloquium Series is part of the Centre’s larger objective of expanding opportunities to foster conversations around health inequities, particularly those relating to gender and its intersections with other sources of structural inequality. The talks cover a range of health concerns (sexual and reproductive health, nutrition, maternal and adolescent health) and multiple axes of disadvantage (gender, caste, migrant status, tribal status, disability, etc.). Invited speakers come from a mix of research, policy, advocacy, and practice backgrounds.
Recordings: https://www.youtube.com/playlist?list=PLI_PWXNhdaCiLmkbTocl55odIzajTiLEM
The Team
- Professor and Director
- Prof. Gita SenDistinguished Professor and Senior Advisor
- Deputy Director
- Research Scientist and Assistant Professor
- Dr Anuradha SreevathsaConsultant
- Ms Ketoki BasuConsultant - Finance
- Manager - Operations
- Ms Arunima GhosalResearch Associate
- Research Associate
- Ms Meher SuriConsultant
- Research Scientist
- Ms. Shanthi Suraj ShettyAdministrative & Finance Officer
- Dr Keerthana AnilkumarConsultant
- Dr Prateek RathiConsultant
- Dr Gayatri MenonConsultant
Public Health Foundation of India
Epidemic Diseases Hospital Compound
Old Madras Road
Indiranagar
Bangalore – 560038
Phone: +080-29710403
About Dr. Ramalingaswami
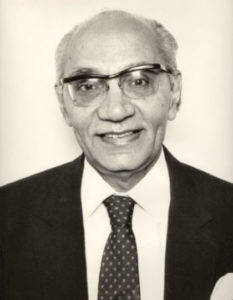 Born on August 8, 1921, Professor Vulimiri Ramalingaswami’s illustrious medical career spanned over half an extremely eventful century. Starting as a Clinical Research Officer at the Nutrition Research Laboratory in Coonoor in 1947, Professor Ramalingaswami went on to become the Director of the All-India Institute of Medical Sciences (1969-79) and the Director General of the Indian Council of Medical Research (1979-1986). He continued to be a National Research Professor until his death on May 28, 2001. Along the way, he garnered several honours, including the Founding Fellow of the Indian Academy of Medical Sciences; Fellow, Royal College of Physicians; Honorary Fellow, American College of Physicians; and Fellow, Royal Society of London, among others. He received numerous awards, including the Padma Shri and Padma Bhushan.
Born on August 8, 1921, Professor Vulimiri Ramalingaswami’s illustrious medical career spanned over half an extremely eventful century. Starting as a Clinical Research Officer at the Nutrition Research Laboratory in Coonoor in 1947, Professor Ramalingaswami went on to become the Director of the All-India Institute of Medical Sciences (1969-79) and the Director General of the Indian Council of Medical Research (1979-1986). He continued to be a National Research Professor until his death on May 28, 2001. Along the way, he garnered several honours, including the Founding Fellow of the Indian Academy of Medical Sciences; Fellow, Royal College of Physicians; Honorary Fellow, American College of Physicians; and Fellow, Royal Society of London, among others. He received numerous awards, including the Padma Shri and Padma Bhushan.
Professor Ramalingaswami’s contributions to medical research are well-documented, in areas ranging from anaemia, protein-energy malnutrition and nutritional pathologies to liver disease, cardiovascular disease and iodine deficiency disorders. Over time, his interest in and understanding of the social determinants of health increasingly informed his research and writing. In ‘Anatomy of Hunger’, a conference paper he wrote in 1976, he speaks of the ‘chronic or endemic hunger and malnutrition which are woven into the complex social texture of under-development’. His views were profoundly impacted by his visit in 1967 to famine-torn Bihar as well as districts of Orissa; and later in the Bangladeshi refugee camps in 1971-72. Later he was involved in mobilising the response to the Bhopal gas tragedy and the outbreak of bubonic plague in Maharashtra and Gujarat in 1994. These experiences built his understanding of the genesis of disease and the need of a strong and resilient health system to mitigate the worst impacts of health disasters.
Professor Ramalingaswami was truly a leader in his field, who in turn mentored and groomed several others in the next generation. His spirit of lively curiosity, commitment to excellence and scholarship, accompanied by a deep awareness of social inequalities and the need to redress them, guides the Ramalingaswami Centre on Equity and Social Determinants of Health.
Rajiv Mehrotra, television anchor and reporter in conversation with Prof. Ramalingaswami.
https://www.youtube.com/watch?v=xFszfmpFGV8
The main image of the centre – Photo by @arjun.swaminathan